
10 Molecular Mechanisms Underlying Allergic Diseases
An allergic reaction occurs when the immune system overreacts to a normally harmless substance, known as an allergen, triggering a cascade of immune responses that result in various clinical symptoms. Allergens can be found in common substances such as pollen, dust mites, animal dander, certain foods, insect venom, and medications.
The process of developing an allergy typically involves sensitization, where the immune system recognizes the allergen as a threat and produces specific antibodies, such as immunoglobulin E (IgE), in response to exposure. Upon subsequent exposure to the same allergen, these antibodies bind to mast cells and basophils, two types of immune cells found in tissues throughout the body.
When the allergen binds to IgE antibodies on the surface of mast cells and basophils, it triggers the release of inflammatory mediators, such as histamine, leukotrienes, and cytokines. These mediators cause the characteristic symptoms of an allergic reaction, which can vary depending on the type of allergen and the individual’s immune response.
Common allergic reactions include:
Respiratory symptoms: Allergic rhinitis (hay fever) causes symptoms such as sneezing, runny or congested nose, itching of the nose and eyes, and watery eyes. Asthma may also be triggered by allergens, leading to wheezing, coughing, chest tightness, and difficulty breathing.
Skin symptoms: Allergic reactions can manifest as eczema (atopic dermatitis), hives (urticaria), or allergic contact dermatitis, resulting in redness, itching, swelling, and rash on the skin.
Gastrointestinal symptoms: Ingestion of certain allergenic foods or medications can lead to symptoms such as nausea, vomiting, abdominal pain, diarrhea, or even anaphylaxis in severe cases.
Anaphylaxis: In some individuals, exposure to an allergen can cause a severe, life-threatening allergic reaction known as anaphylaxis. Symptoms may include difficulty breathing, swelling of the face and throat, rapid heartbeat, drop in blood pressure, loss of consciousness, and shock.
Treatment of allergic reactions typically involves avoiding known allergens whenever possible and using medications such as antihistamines, corticosteroids, decongestants, or epinephrine (in the case of anaphylaxis) to alleviate symptoms. Allergy testing and immunotherapy (allergy shots) may also be recommended to desensitize the immune system and reduce allergic responses over time.
10.1 Allergens in the Singaporean Context
Allergen response in Singapore is notably high, with approximately 70% of individuals experiencing allergic sensitization to various allergens. Among allergic subjects, a significant proportion, approximately 95%, exhibit allergic reactions specifically to house dust mites, which are one of the most prevalent indoor allergens in Singapore and globally. House dust mites are microscopic arthropods commonly found in household dust, bedding, upholstery, and carpets, and their allergenic proteins can trigger allergic rhinitis, asthma, and eczema in sensitized individuals.
However, it’s worth noting that not all allergic subjects in Singapore have a house dust mite allergy. Approximately 5% of allergic individuals do not exhibit allergic sensitization to house dust mites, suggesting that other allergens, such as pollen, mold spores, animal dander, or specific food allergens, may be responsible for their allergic symptoms.
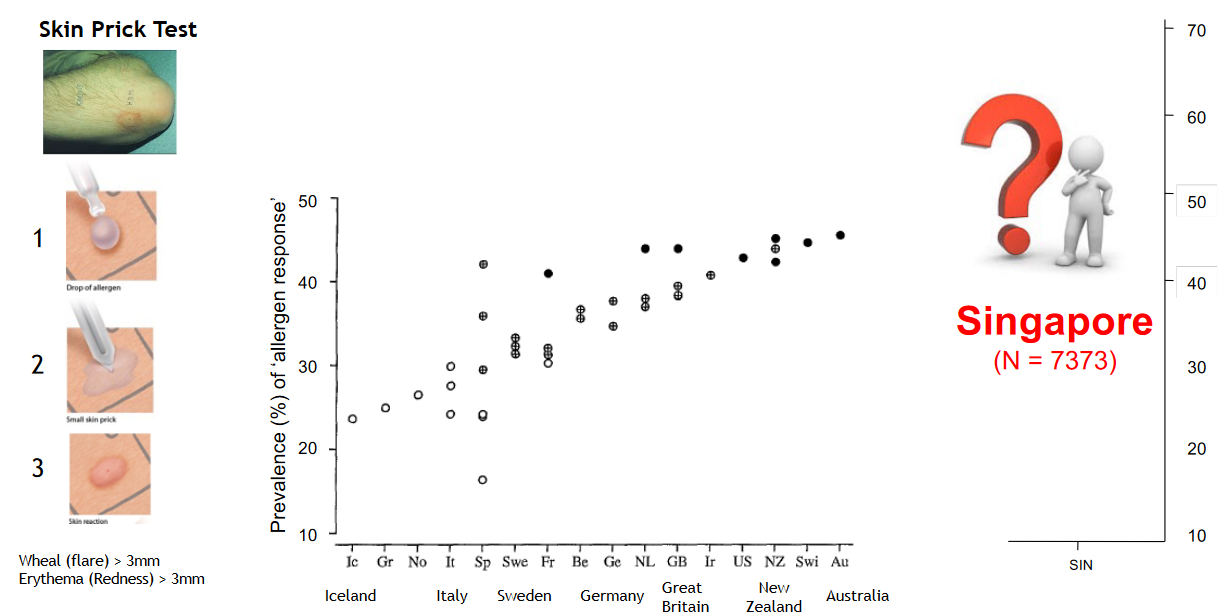
Skin prick tests are commonly used by allergists and immunologists in Singapore to diagnose allergic sensitization and identify specific allergens responsible for triggering allergic reactions in patients. During the test, small amounts of common allergens are applied to the skin’s surface, typically on the forearm or back, and the skin is pricked or scratched to allow the allergens to enter the skin’s outer layer. If a person is allergic to a particular allergen, they may develop a small, raised bump (wheal) and surrounding redness (flare) at the test site within 15 to 20 minutes.
10.1.1 Costs of Allergens

Allergen response in Singapore not only manifests as sensitization but also results in clinical diseases such as allergic rhinitis, asthma, and eczema, imposing a significant economic burden on individuals and society. With an overall allergy prevalence of 50%, approximately one in every two individuals in Singapore experiences allergic sensitization or related clinical symptoms. House dust mite (HDM) allergy is particularly prevalent, contributing to the development of allergic rhinitis, asthma, and eczema in affected individuals.
The clinical impact of allergen response is substantial, leading to various allergic conditions that significantly affect individuals’ quality of life and productivity. Allergic rhinitis, asthma, and eczema can cause symptoms such as nasal congestion, sneezing, wheezing, coughing, skin rashes, and itching, impairing daily activities and sleep quality.
Furthermore, the economic burden of allergic diseases, particularly asthma and eczema, is considerable in Singapore. Asthma imposes an annual economic burden of approximately US$1.50 billion, with productivity losses accounting for 79% of the total cost. Eczema also incurs significant costs per patient, ranging from USD 6,651 to 14,335, depending on the severity of the condition, from mild to severe.
10.1.2 Reasons for High Allergy Rates
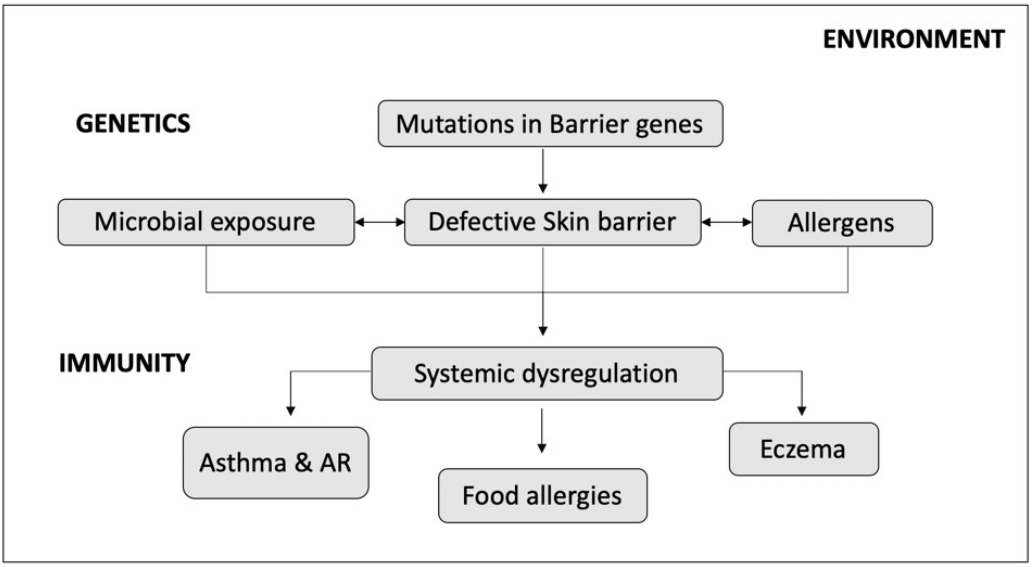
The high rate of allergic sensitization and disease in Singapore, as in many other parts of the world, is the result of a complex interaction of multiple risk factors involving genetic predisposition, environmental exposures, lifestyle factors, and immunological mechanisms.
Genetic Predisposition: Genetic factors play a significant role in predisposing individuals to allergic diseases. Certain genetic variations and polymorphisms influence immune responses, leading to an increased susceptibility to allergic sensitization and the development of allergic conditions such as asthma, allergic rhinitis, and eczema. Individuals with a family history of allergies are at a higher risk of developing allergic diseases themselves.
Environmental Exposures: Environmental factors play a crucial role in allergic sensitization and disease development. Exposure to allergens such as house dust mites, pollen, mold spores, pet dander, and certain foods can trigger allergic reactions in susceptible individuals. Urbanization, industrialization, indoor air pollution, and changes in lifestyle habits may contribute to increased exposure to allergens and pollutants, further exacerbating allergic conditions.
Immunological Dysregulation: Allergic diseases result from dysregulated immune responses to allergens, characterized by an imbalance between pro-inflammatory and anti-inflammatory pathways. In allergic individuals, the immune system overreacts to harmless substances, producing excessive levels of immunoglobulin E (IgE) antibodies and inflammatory mediators such as histamine, cytokines, and leukotrienes, leading to the characteristic symptoms of allergic reactions.
Hygiene Hypothesis: The hygiene hypothesis posits that reduced exposure to microbial pathogens and infections during early childhood may contribute to an increased risk of allergic diseases. Improved sanitation, hygiene practices, and reduced exposure to microbes in modern urban environments may alter immune development and increase susceptibility to allergic sensitization and disease.
Diet and Lifestyle Factors: Dietary factors, lifestyle habits, and environmental exposures can influence immune function and allergic responses. Changes in dietary patterns, including increased consumption of processed foods, allergenic foods, and food additives, may contribute to the rising prevalence of food allergies and intolerances. Lifestyle factors such as sedentary behavior, obesity, stress, and air pollution can also exacerbate allergic symptoms and increase the risk of developing allergic diseases.
10.1.2.1 Allergens and the Environment
In tropical-urban settings like Singapore, the unique allergen environment influences the prevalence and severity of allergic diseases. One notable characteristic is the extreme dominance of a single allergen, particularly house dust mites, which are ubiquitous in indoor environments and a major trigger for allergic reactions.
Exposure to high levels of allergens such as dust mites, pollen, mold spores, and pet dander in the environment can lead to allergic sensitization, where the immune system mounts an abnormal response to otherwise harmless substances. This dysregulated immune response is characterized by the production of allergen-specific IgE antibodies and the activation of inflammatory pathways, leading to allergic symptoms such as asthma, allergic rhinitis, and eczema.
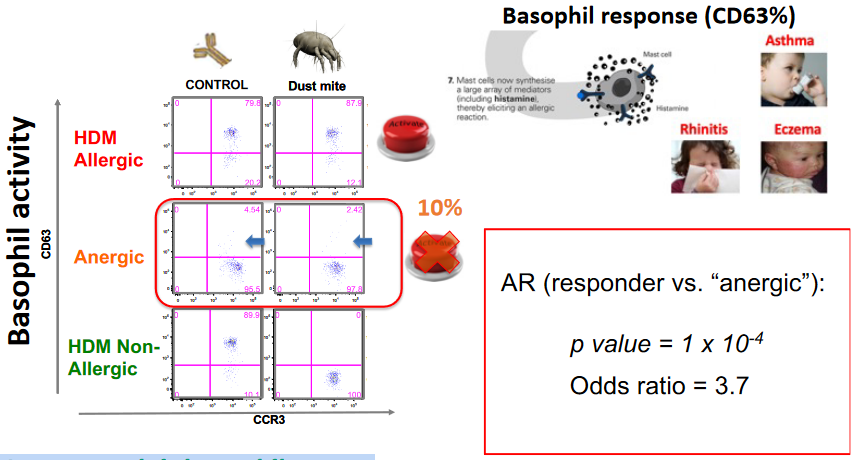
Basophil anergy, a state of hypo-responsiveness or unresponsiveness of basophils to allergen stimulation, is a phenomenon observed in some individuals with allergic diseases. Exploiting basophil anergy for allergen desensitization is a potential strategy in allergen immunotherapy, a treatment approach aimed at modulating the immune system’s response to allergens and reducing allergic symptoms and severity.
Allergen immunotherapy involves the administration of gradually increasing doses of allergen extracts to allergic individuals, leading to immune tolerance and reduced allergic reactivity over time. By inducing immune tolerance and desensitizing basophils and other effector cells involved in allergic responses, allergen immunotherapy can alleviate allergic symptoms, improve quality of life, and potentially prevent disease progression.
10.2 Characterizing Immunopathobiology of Allergens
One key aspect of molecular immunopathobiology is the identification and characterization of molecular allergen responses. This involves the analysis of specific allergenic proteins or molecules that trigger allergic reactions in sensitized individuals. Techniques such as skin prick tests (SPT) and basophil activation tests (BAT) are utilized to assess the allergic response to different allergens and determine the presence of allergen-specific IgE antibodies, which play a central role in allergic sensitization and immune activation.
Furthermore, understanding the immune dysregulation underlying allergic diseases is crucial for targeted therapeutic interventions. Immune dysregulation in allergies involves aberrant immune responses characterized by the activation of inflammatory pathways, dysregulated cytokine production, and impaired regulatory mechanisms. By characterizing the molecular pathways involved in immune dysregulation, researchers can identify potential targets for novel immunomodulatory therapies aimed at restoring immune balance and attenuating allergic inflammation.
Barrier dysfunction is another critical aspect of allergic diseases, particularly in conditions such as atopic dermatitis and allergic asthma. Impaired skin and mucosal barriers compromise their protective function, allowing allergens to penetrate and trigger immune responses. Molecular characterization of barrier dysfunction involves studying the integrity of the skin and mucosal barriers, as well as the role of epithelial cells, tight junctions, and antimicrobial peptides in maintaining barrier function.
10.3 Allergic Rhinitis (professor’s research)
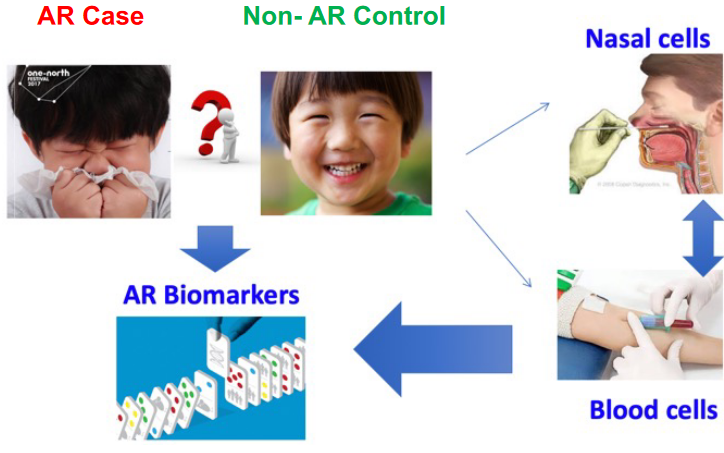
Allergic rhinitis is characterized by a dysregulated immune response and alterations in nasal epithelial barrier function, leading to variable gene expression patterns that contribute to the pathogenesis of the disease.
10.3.1 Findings
One notable finding was the strong enrichment of genes associated with type 2 inflammation, a hallmark of allergic diseases such as AR. These genes represent promising targets for therapeutic intervention aimed at modulating the inflammatory response underlying AR pathogenesis.
Additionally, replication of AR candidate genes in the BAMSE (Swedish birth cohort) study revealed that a significant proportion of identified candidate genes were also associated with allergic rhinitis in the Swedish population. Among these candidate genes, the majority highlighted the role of eosinophils in disease pathogenesis, suggesting eosinophils as potential targets for therapeutic intervention in AR. Eosinophils are immune cells implicated in allergic inflammation and are known to contribute to tissue damage and inflammation in AR.
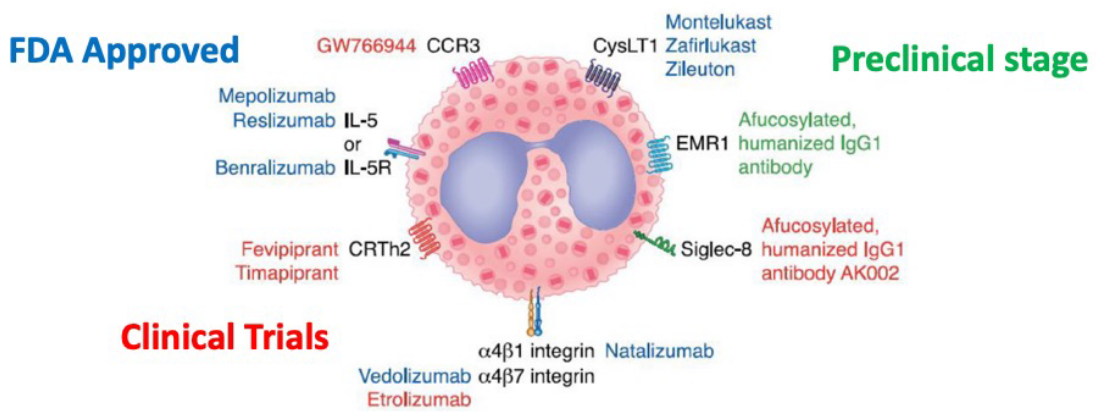
Furthermore, targeting eosinophils for therapeutic options and molecular candidates represents a promising strategy for AR treatment. Many of the significant AR candidate genes identified in the study are already recognized therapeutic targets, indicating the potential for further exploitation of eosinophil-targeted therapies in AR management. By modulating eosinophil function and activity, these therapies aim to alleviate allergic inflammation and improve clinical outcomes in AR patients.
10.4 Allergic Dermatitis
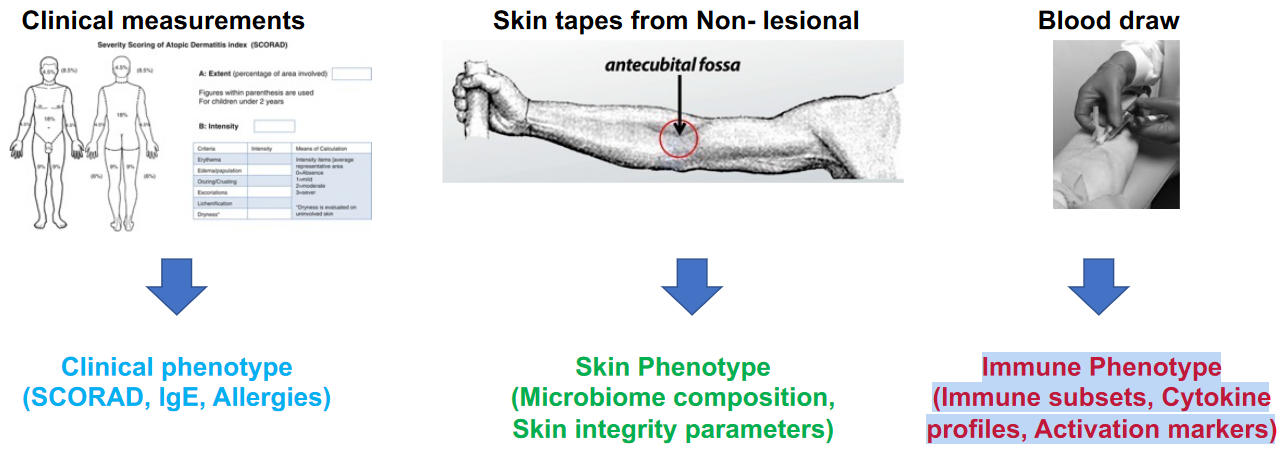
Clinical measurements, such as SCORAD (Scoring Atopic Dermatitis) scores, serum IgE levels, and allergies, provide insights into the severity and allergic status of AD patients compared to non-AD individuals. AD patients typically exhibit higher SCORAD scores, elevated IgE levels, and increased prevalence of allergies compared to non-AD individuals.
Skin tapes collected from non-lesional areas allow for the assessment of skin phenotype, including microbiome composition and skin integrity parameters. Studies have revealed differences in the microbiome composition of non-lesional skin between AD patients and non-AD individuals, with alterations in microbial diversity and abundance observed in AD patients. Additionally, skin integrity parameters such as transepidermal water loss (TEWL) and skin barrier function may be compromised in AD patients, contributing to susceptibility to microbial colonization and inflammation.
Blood draws facilitate the evaluation of immune phenotype, including immune subsets, cytokine profiles, and activation markers, which further elucidate the underlying immunological differences between AD and non-AD individuals. AD patients often exhibit alterations in immune cell subsets, such as increased frequencies of T helper 2 (Th2) cells and decreased regulatory T cells (Tregs), contributing to immune dysregulation and allergic inflammation. Additionally, elevated levels of pro-inflammatory cytokines, such as interleukin-4 (IL-4), IL-13, and tumor necrosis factor-alpha (TNF-α), are commonly observed in AD patients, reflecting ongoing immune activation and inflammation in the skin.
10.4.1 Skin Barrier Dysfunction

Skin tape samples collected from non-lesional areas reveal variations in the microbiome profile between atopic dermatitis (AD) patients and non-AD individuals, with a notable difference in species composition. In AD patients, the microbiome profile of non-lesional skin exhibits a variable composition of microbial species compared to non-AD individuals. These variations may include differences in the relative abundance and diversity of bacterial, fungal, and other microorganisms inhabiting the skin.
10.4.1.1 Effects
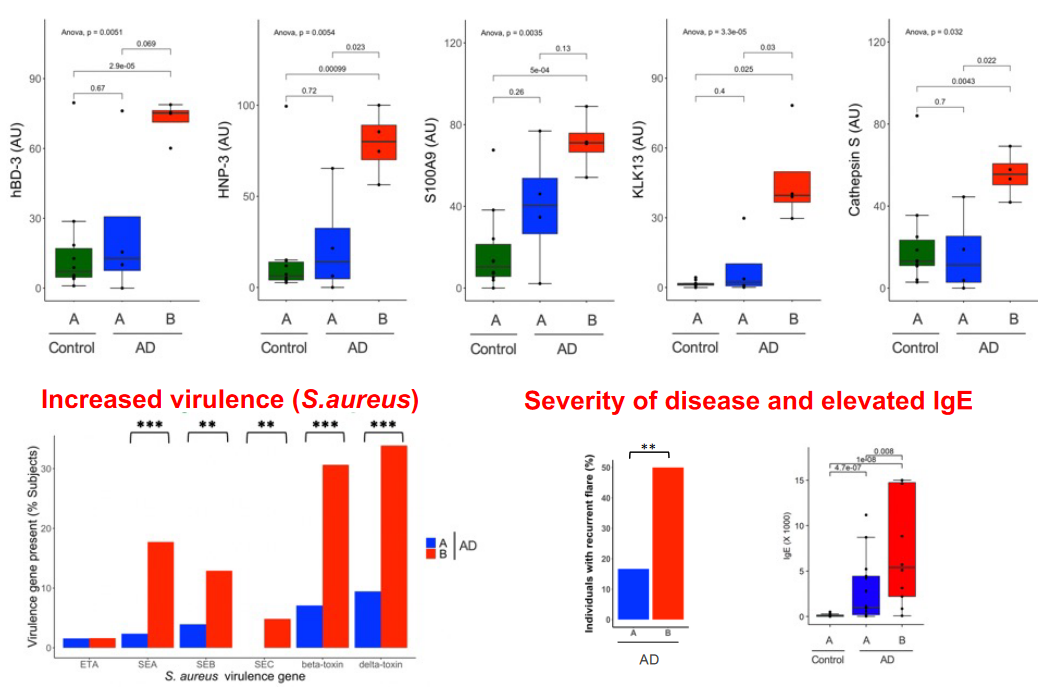
Skin barrier dysfunction associated with alterations in the microbiome profile, particularly increased virulence of Staphylococcus aureus, can exacerbate the severity of atopic dermatitis (AD) and elevate serum IgE levels.
Increased Virulence of Staphylococcus aureus: Staphylococcus aureus colonization is often observed in AD patients and can contribute to skin barrier dysfunction. This bacterium produces virulence factors such as toxins and enzymes that can disrupt the skin barrier by damaging epithelial cells, compromising tight junctions, and triggering inflammation. These virulence factors may exacerbate skin inflammation and contribute to the development of AD lesions, leading to increased disease severity and prolonged episodes of exacerbation.
Severity of Disease and Elevated IgE: Skin barrier dysfunction in AD allows for increased penetration of allergens, microbial antigens, and irritants, leading to heightened immune responses and elevated serum IgE levels. Disruption of the skin barrier allows allergens and microbial components to penetrate deeper into the skin, triggering immune responses and inflammatory reactions. This dysregulated immune response further compromises the skin barrier, creating a cycle of inflammation and barrier dysfunction. Elevated IgE levels are often associated with increased disease severity in AD and may contribute to allergic sensitization and exacerbation of symptoms.
Skin barrier dysfunction is closely associated with immune dysregulation and inflammation in conditions such as atopic dermatitis (AD). When the skin barrier is compromised, it allows for the entry of allergens, pathogens, and other environmental irritants, triggering an immune response characterized by inflammation.
10.5 Single Cell Technology
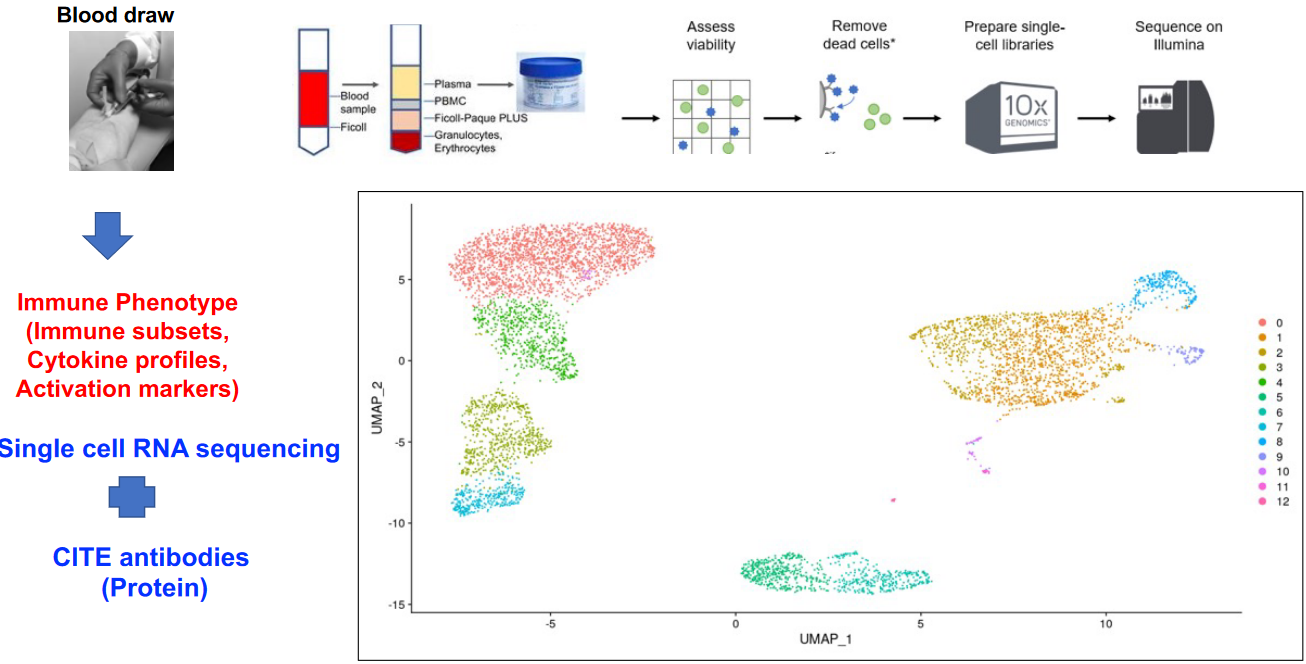
Single-cell technology has emerged as a powerful tool for addressing immune heterogeneity. Traditional bulk analysis methods provide average measurements across populations of cells, masking the diversity and complexity inherent within immune cell populations. Single-cell technologies, on the other hand, enable the high-resolution profiling of individual immune cells, allowing researchers to capture the full spectrum of cellular diversity within a sample.
10.5.1 Findings
10.5.1.1 Finding 1

Monocyte-mediated inflammation has emerged as a potential contributor to the pathophysiology of atopic dermatitis (AD), particularly in individuals with Dermotype B-associated AD. Dermotype B is characterized by specific clinical and molecular features, including alterations in skin barrier function, immune dysregulation, and microbial dysbiosis. Recent research efforts are focused on validating the association between monocyte-mediated inflammation and Dermotype B-associated AD pathophysiology.
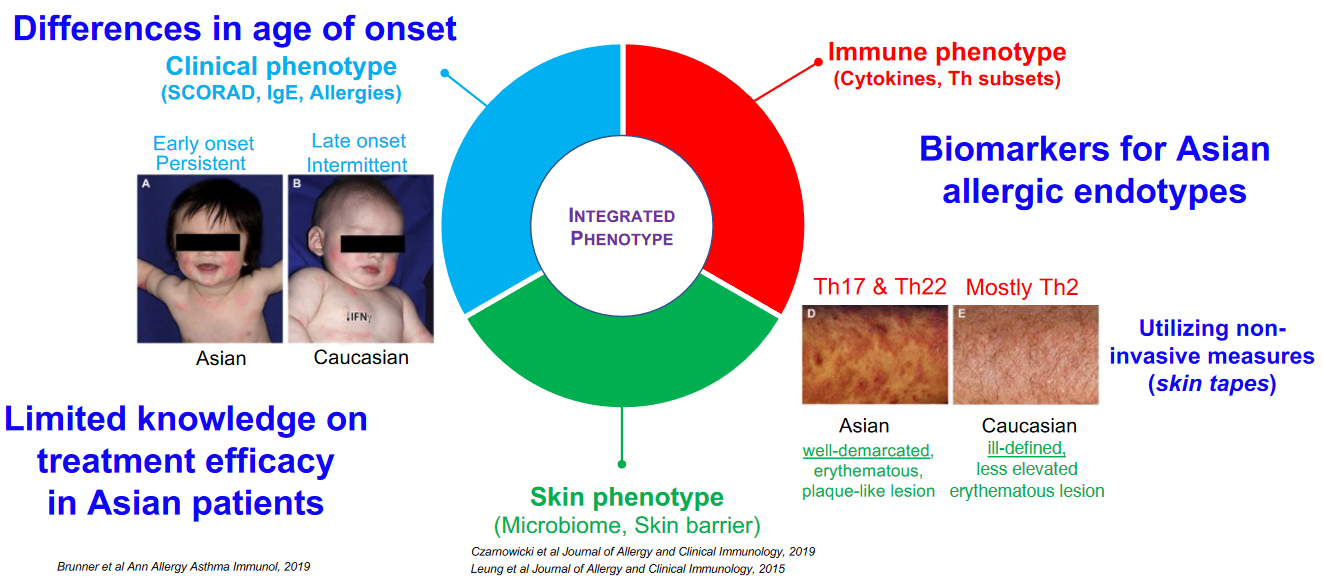
Variances exist in the age of onset, treatment responses, and underlying mechanisms across different demographic groups. In the context of Asian patients, there’s a notable gap in understanding treatment efficacy compared to other populations. The effectiveness of certain therapies may differ, necessitating tailored approaches to management. Moreover, the identification of biomarkers specific to allergic endotypes prevalent in Asian populations remains a challenge. These biomarkers are crucial for stratifying patients based on their underlying disease mechanisms and predicting treatment responses accurately.
10.6 Endotypes

Allergies manifest through various specific pathomechanisms, which are referred to as endotypes. These endotypes represent distinct biological mechanisms underlying allergic diseases and can influence disease presentation, severity, and response to treatment. For example, some individuals may have allergies driven primarily by IgE-mediated immune responses to specific allergens, while others may experience symptoms due to non-IgE-mediated mechanisms such as T-cell mediated inflammation or epithelial barrier dysfunction.
10.6.1 Type 2 Inflammatory Subsets
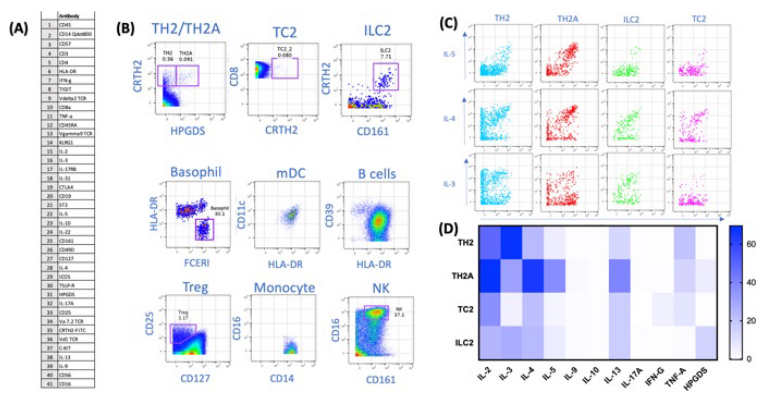
In the context of Type 2 inflammatory subsets, such as those seen in allergic diseases like asthma and atopic dermatitis, functional cytokine characterization upon stimulation plays a crucial role. By analyzing the cytokine profiles produced by immune cells upon activation, healthcare providers can gain insights into the specific inflammatory pathways driving the disease. This information is invaluable for targeted therapy, as it allows for the selection of treatments that directly inhibit or modulate these inflammatory pathways. Additionally, monitoring treatment response through cytokine profiling enables clinicians to assess the effectiveness of therapy and adjust treatment strategies as needed.
Moreover, matching the molecular endotype of the disease to its clinical presentation is essential for personalized medicine approaches. By identifying the specific molecular pathways driving the disease in an individual patient, healthcare providers can tailor treatment plans to target those pathways specifically.
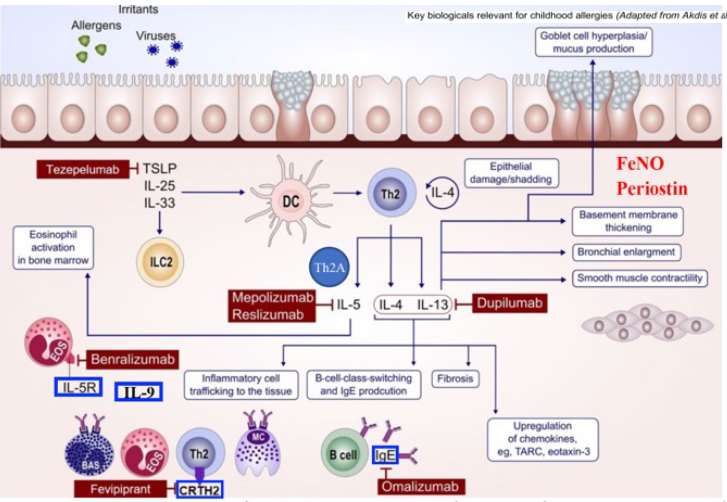
One strategy involves resolving clinical phenotypes into molecular endotypes, which represent distinct underlying biological mechanisms driving the disease. By identifying these molecular endotypes and associated biomarkers, healthcare providers can tailor treatment strategies to target the specific pathophysiological pathways active in each individual patient.
To achieve this, comprehensive characterization of patients using advanced molecular profiling techniques, such as genomics, transcriptomics, proteomics, and metabolomics, is necessary. These techniques can identify molecular signatures, including genetic variants, gene expression patterns, protein markers, and metabolic profiles, that correlate with different clinical phenotypes and treatment responses. Additionally, integrating data from large-scale omics studies with clinical data, such as symptom severity, disease progression, and treatment outcomes, can facilitate the discovery of predictive biomarkers and therapeutic targets.
Furthermore, incorporating machine learning and artificial intelligence algorithms into clinical practice can help analyze complex omics data and identify patterns associated with treatment response.